Treatment For Special Populations
Pregnant Women
Treatment for Pregnant women:
Current clinical recommendations for pregnant people with OUD include medication for opioid use disorder (MOUD) rather than supervised withdrawal due to a higher likelihood of better outcomes and a reduced risk of relapse (CDC, November 2022).
- Healthcare providers and pregnant people with OUD should work together to manage medical care during pregnancy and after delivery.
- Coordination of care between a prenatal care provider and a specialist with expertise in opioid use helps avoid problems for pregnant people and their babies.
- Methadone and buprenorphine are first-line therapy options for pregnant people with OUD, along with behavioral therapy and medical services.
- While some treatment centers use naltrexone to treat OUD in pregnant people, information on its safety during pregnancy is limited.
- If a woman is stable on naltrexone before pregnancy, continuing naltrexone treatment during pregnancy should involve a careful discussion between the provider and the patient.
Infants
Infants born to women who use opioids are likely to have physiological disturbances and low birth weight (Developing Brain Institute, 2022).
- Using opioids during pregnancy may cause early labor, fetal distress, or miscarriage.
- Pregnant women need supervised withdrawal.
- Babies should be monitored for Neonatal Abstinence Syndrome (NAS) and be referred to services, as needed.
- Breastfeeding is usually encouraged for newborns with NAS.
- SAMHSA’s National Helpline at 1 – 800-662-HELP (4357) provides guidelines for managing the care of infants with long-term opioid exposure during pregnancy.
More recently, infants born to moms using fentanyl may have small heads, webbed fingers, genital abnormalities, and other peculiarities (Edwards, NBC News, 2023, Dec. 5). Doctors have found, in a dozen cases, a probable association between fentanyl use and these babies’ development and have ruled out genetic causes but have not been able to establish a causal relationship with fentanyl truly. More studies are needed to determine if there are other agents or a mixture of them and other causes which could explain these defects. In the meantime, pregnant mothers are advised not to use fentanyl.
Fentanyl exposure during pregnancy possibly linked
to new medical syndrome in babies.
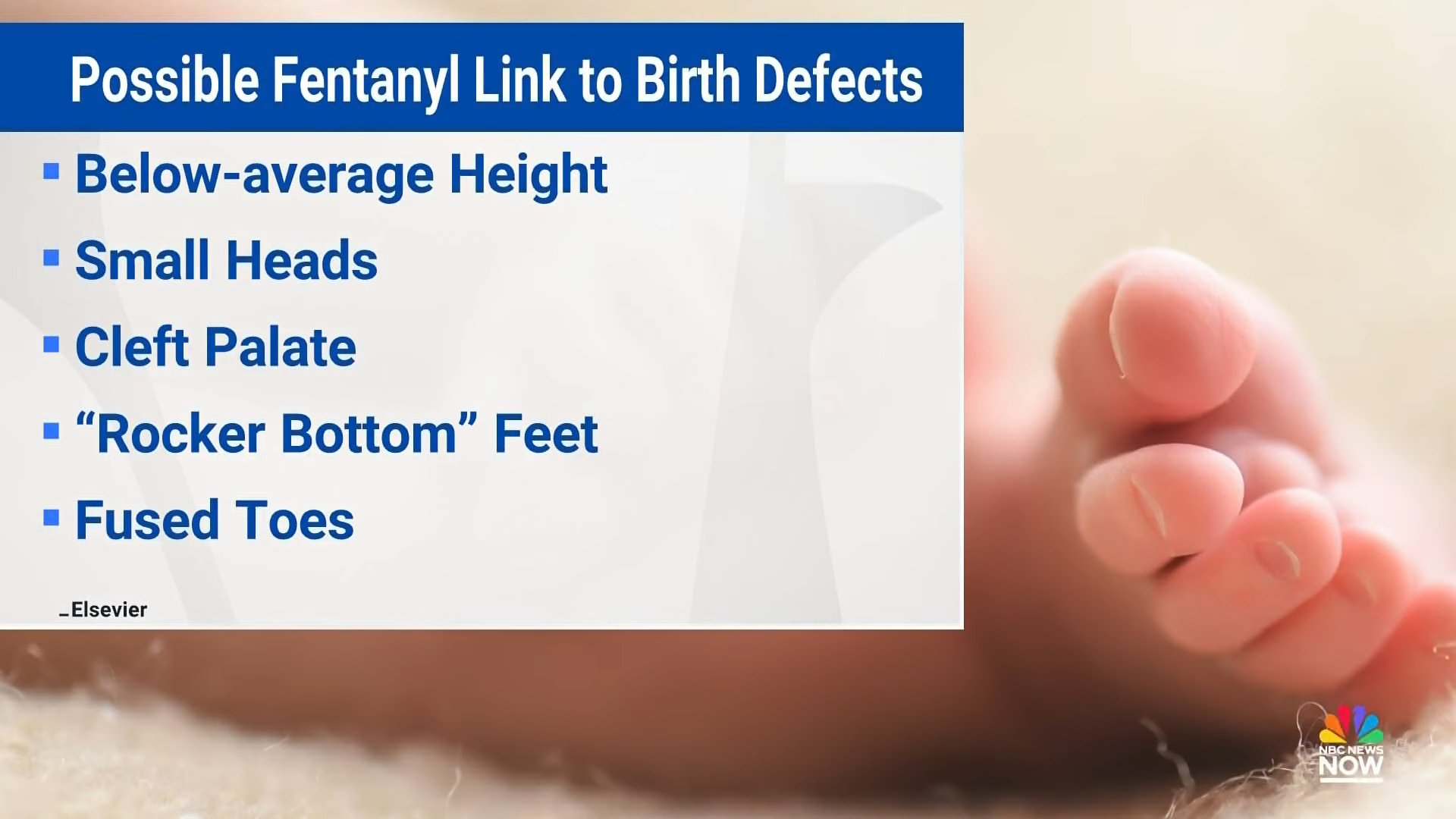
NBC News | https://youtu.be/zgF2CPtP7bA
Veterans
Factors that Can Affect Veterans
- Opioid misuse issues
- Chronic pain
- Stress
- Traumatic experiences
Veterans benefit from services delivered by individuals who share key experiences or similar backgrounds (Peer Support). They may need help or other interventions to connecting to the Veterans Health Administration. Services for veterans should incorporate the perspectives and voices of veterans with the lived experience of substance use.
Veteran’s Crisis Line: 1 – 800-273‑8255
Peer Support Specialists
SAMHSA (n.d.) explains peer recovery support services, which can be an alternative or addition to clinical assistance. The peer recovery coaches work in various venues: recovery community centers, drug courts, hospital emergency departments, homeless shelters, and other areas. They are active in outreach and building trust with their clients — offering an example of hope, positively impacting treatment retention, decreased need for emergency services, reduced substance use, greater housing stability, and other positive goals.
Peer recovery specialists are helpful for those coming off opioids with issues of addiction, mental health, and other life challenges. There are two types: recovery coaches and peer specialists. Recovery coaches are formally trained professionals, and peer specialists are trained but have lived experience with addiction. Recovery coaches are typically trained professionals generally with a background in counseling, social work, or related fields, according to Ventusrex (2023, Feb. 2).
Peer specialists provide hope, encouragement, and practical support to individuals in recovery, such as helping them access resources and services and build a support network. Details about the 60-hour training program are at: pss.unc.edu/certification.NC Certified Peer Support Specialist Program, School of Social Work, The University of North Carolina at Chapel Hill, 325 Pittsboro Street, Campus Box #3550, Chapel Hill, North Carolina 27599 – 3550. Source: Ventusrex. https://www.ventusrex.com/state-peer-certification-requirements/north-carolina/
What Does a Peer Specialist Do?

Those Released from Prison
There are roughly 2 million people in prisons and jails at any given time in the United States, but fewer than 1% of jails and prisons in the U.S. offer MAT with MOUD for OUD.
With the risk of overdose during the first two weeks post-release nearly 40 times higher among formerly incarcerated individuals compared to the general public, access to MOUD within the justice system and expedited transitions to treatment in the community is critical. Jail-based MAT programs can take many different forms and can be implemented gradually based on the resources and capacity of the individual detention center.
Resources:
- Addiction Treatment for Incarcerated Persons — North Carolina Opioid Settlements (ncopioidsettlement.org)
- Methadone and MAT in Prisons and Jails
- Formerly Incarcerated Transition (FIT) Program connects formerly incarcerated individuals who have a chronic disease, mental illness and/or substance use disorder with health care services and other resources.
- Reservoir of Hope provides housing for men who have recently been released, wrap-around services, and mental health counseling.
- Religious Coalition for Non-Violent Durham. Drew Doll, Reentry and Reconciliation Coordinator. reentry@nonviolentdurham.org
- Coming Home — A Justice-Involved Permanent Supportive Housing Program. Email: ncreferral@rhd.org. Phone: (919) 755‑1335.
- Local Reentry Council. 326 East Main Street, Durham, North Carolina 27701. Phone: (919) 560‑7589. Email: durhamlrc@dconc.gov. Website: https://www.dconc.gov/county-departments/departments-f‑z/justice-services/durham-local-reentry-council
Addressing Barriers to MOUDs Faced by People in Incarceration
Factors that Compound the Problem
- A lack of in-prison substance misuse treatment feeds the growing opioid crisis.
- Former opioid users in prison may have developed a lower tolerance to the drug.
As of 2021, the Durham County Detention Center is now just one of three county detention centers in North Carolina to be ACA-certified, joining facilities in Mecklenburg and New Hanover counties. Performance-Based Health Care Standards for Adult Local Detention Facilities, Fourth Edition, is another aspect of accreditation. It is unknown if ACA has accredited the health care at these facilities, which is especially important because it is the interface crucial for prisoners’ health when they leave. If they have received MOUD treatment inside, there should be a link to resources outside to ensure follow-up and medication treatment is not stopped.
Those who run jails and detention facilities, including juvenile facilities, should be sure they do the following things:
- In intake, assess mental health, especially suicide risk and follow up. Be sure there is sufficient staffing to allow for the follow-up.
- Provide mental health services.
- Perform MOUD for those with substance misuse.
- Promote visitation.
- Encourage communication with the inmates/juveniles.
For returning citizens:
- Provide housing, jobs, and healthcare linkages, including mental health services, before the person leaves prison, and set up mental health follow-through.
- Remind them that alcohol intensifies the impact of substance misuse and is likely to kill them.
- Peer support is vital. Make the link during the incarceration and follow through to see that it is followed on the outside.
- For juveniles estranged from their families, encourage the development of a mentor relationship so the juvenile has someone to turn to if things are problematic in their housing and care arrangements.
- Establish these links while the person is still incarcerated.
Narcan vending machines now in two Durham County buildings as part of fight against opioid-related deaths

ABC11 Eyewitness News
ABC11 Eyewitness News | https://www.youtube.com/watch?v=LAQfgG53y_o
Opioid use disorder treatment in jails making strides in North Carolina.
Framing MOUD in jails as an Americans with Disabilities Act issue is prompting a shift in how the treatment is managed, with jails now more willing to sort out the logistics. Crumpler September 27, 2022. NC Health News.
North Carolina Opioid Settlements, North Carolina has implemented a strategy to support evidence-based addiction treatment, including Medication-Assisted Treatment (MAT) with at least one FDA-approved opioid agonist for persons who are incarcerated in jail or prison. The strategy aims to increase the availability of MAT with FDA-approved medications, such as buprenorphine, within the justice system. Studies have shown that MAT reduces criminal activity, overdose risk, the spread of costly infectious diseases, and recidivism. The North Carolina Department of Public Safety and the Department of Health and Human Services plans to pilot MAT programs.
Laws Helping to Fight Injustices
Your Right to Methadone & Buprenorphine in New York Jails & Prisons Explainer Video

Source: Legal Action Center
Resources
Your Right to Methadone and Buprenorphine
in New York Jails & Prisons
SAMHSA National Helpline 1 – 800-662‑4357
Principles of Effective Treatment
Click on each statement for details.
1. Addiction is a complex but treatable disease that affects brain function and behavior.
Because drug misuse and addiction — both of which are mental disorders — often co-occur with other mental illnesses, patients presenting with one condition should be assessed for the other(s). And when these problems co-occur, treatment should address both (or all), including the use of medications, as appropriate.
2. No single treatment is appropriate for everyone.
Treatment varies depending on the type of drug and the characteristics of the patients. Matching treatment settings, interventions, and services to an individual’s particular problems and needs is critical to his or her ultimate success in returning to productive functioning in the family, workplace, and society.
3. Treatment needs to be readily available.
Because drug-addicted individuals may be uncertain about entering treatment, taking advantage of available services the moment people are ready for treatment is critical. Potential patients can be lost if treatment is not immediately available or readily accessible. As with other chronic diseases, the earlier treatment is offered in the disease process, the greater the likelihood of positive outcomes.
4. Effective treatment attends to multiple needs of the individual, not just his or her drug misuse.
To be effective, treatment must address the individual’s drug use and any associated medical, psychological, social, vocational, and legal problems.
5. Remaining in treatment for an adequate period of time is critical.
The appropriate duration for an individual depends on the type and degree of the patient’s problems and needs. Research indicates that most addicted individuals need at least three months of treatment to reduce or stop their drug use significantly and that the best outcomes occur with longer durations of treatment. Recovery from drug addiction is a long-term process and frequently requires multiple episodes of treatment. As with other chronic illnesses, relapses to drug misuse can occur and should signal a need for treatment to be reinstated or adjusted. Because individuals often leave treatment prematurely, programs should include strategies to engage and keep patients in treatment.
6. Behavioral therapies — including individual, family, or group counseling — are the most commonly used forms of drug misuse treatment.
The types of treatment services include:
- Individual counseling. One-on-one counseling to explore personal problems that an individual may not be comfortable discussing in a group setting.
- Group counseling
- Educational services
- Vocational services
- Life skills
- Mental health treatment
- Family services
- Continuing care
7. Medications are an important element of treatment for many patients, especially when combined with counseling and other behavioral therapies.
Methadone, buprenorphine, and naltrexone (including a new long-acting formulation) are effective in helping individuals addicted to heroin or other opioids stabilize their lives and reduce their illicit drug use. Acamprosate, disulfiram, and naltrexone are medications approved for treating alcohol dependence. For persons addicted to nicotine, a nicotine replacement product (available as patches, gum, lozenges, or nasal spray) or an oral medication (such as bupropion or varenicline) can be an effective component of treatment when part of a comprehensive behavioral treatment program.
8. An individual’s treatment and services plan must be assessed continually and modified as necessary to ensure that it meets his or her changing needs.
A patient may require varying combinations of services and treatment components during treatment and recovery. In addition to counseling or psychotherapy, a patient may require medication, medical services, family therapy, parenting instruction, vocational rehabilitation, and/or social and legal services. For many patients, a continuing care approach provides the best results, with the treatment intensity varying according to a person’s changing needs.
9. Many drug-addicted individuals also have other mental disorders.
Substance use and addiction can contribute to the development of mental illness. Substance use can lead to changes in some of the same brain areas that are disrupted in other mental disorders, such as schizophrenia, anxiety, mood, or impulse-control disorders.
10. Medically assisted detoxification is only the first stage of addiction treatment and by itself does little to change long-term drug misuse.
Although medically assisted detoxification can safely manage the acute physical symptoms of withdrawal and can, for some, pave the way for effective long-term addiction treatment, detoxification alone is rarely sufficient to help addicted individuals achieve long-term abstinence. Thus, patients should be encouraged to continue drug treatment following detoxification. Motivational enhancement and incentive strategies, begun at initial patient intake, can improve treatment engagement.
11. Treatment does not need to be voluntary to be effective.
Sanctions or enticements from family, employment settings, and/or the criminal justice system can significantly increase treatment entry, retention rates, and the ultimate success of drug treatment interventions.
12. Drug use during treatment must be monitored continuously, as lapses during treatment do occur.
Drug use during treatment must be monitored continuously, as lapses during treatment do occur. Knowing their drug use is being monitored can be a powerful incentive for patients and can help them withstand urges to use drugs.
13. Treatment programs should test patients for the presence of HIV/AIDS, hepatitis B and C, tuberculosis, and other infectious diseases, as well as provide targeted risk-reduction counseling, linking patients to treatment if necessary.
Typically, drug misuse treatment addresses some of the drug-related behaviors that put people at risk of infectious diseases. Targeted counseling focused on reducing infectious disease risk can help patients further reduce or avoid substance-related and other high-risk behaviors. Counseling can also help those who are already infected to manage their illness. Moreover, engaging in substance misuse treatment can facilitate adherence to other medical treatments. Substance misuse treatment facilities should provide onsite, rapid HIV testing rather than referrals to offsite testing — research shows that doing so increases the likelihood that patients will be tested and receive their test results. Treatment providers should also inform patients that highly active antiretroviral therapy (HAART) has proven effective in combating HIV, including among drug-abusing populations, and help link them to HIV treatment if they test positive.
Support community efforts to prevent, reduce, and/or eliminate substance misuse
Existing Community Engagement Activates include South Portland (SoPo) Drug-Free Communities Coalition: SoPo Unite and the Cherokee Nation HEAL Initiative (PDF)
Peer Support Specialists (PSS) or peer recovery specialists are people living in recovery with substance/opioid use disorder. A PSS can support an individual with opioid use disorder, either working one-to-one or in a group.
Additional Treatment Resource
Finding High-Quality Treatment
TROSA is an innovative, multi-year residential program that empowers people with substance use disorders to be productive, recovering individuals by providing comprehensive treatment, experiential vocational training, education, and continuing care.
Food, housing, and behavioral/mental
health services are provided at no cost.
1820 James Street
Durham, NC 27707
919 – 419-1059 (Admissions) • https://trosainc.org
If you or a family member needs help with a mental health or substance use disorder, try one of the following:
- Call SAMHSA’s National Helpline at 1 – 800-662-HELP (4357) or TTY: 1 – 800-487‑4889.
- Text your zip code to 435748 (HELP4U).
- Resources for Families Coping with Mental and Substance Use Disorders (SAMHSA)
- Find treatment options at https://findtreatment.gov/.
- Refer to the resource guide for many services around Durham.
Test Your Knowledge (answer yes or no)
1. Opioids change how your brain works.
YES: Addiction causes significant changes in brain chemistry.
2. It’s okay to combine opioids and alcohol as long as it is in very small amounts (less than 1 drink).
NO: Combining any drugs is highly dangerous and unpredictable, especially opioids and alcohol.
3. The FDA has approved three opiate withdrawal medications.
YES: The three main drugs are methadone, buprenorphine, and naltrexone.
4. Everyone has access to opioid treatment.
NO: Everyone should have access to opioid treatment in an ideal situation, but geography and other factors unfortunately limit some people’s access.
5. Treatment should be closely monitored.
YES: It is important to carefully monitor treatment progress and make adjustments accordingly.