Understanding Treatment and Providing Support
OPIOID USE DISORDER is best treated by an integrated health care team that addresses both the patient’s physical and mental health needs. Effective care will include proper communication among team members, respect for the opinions of all healthcare providers involved, and prioritize patient involvement in treatment decisions.
Opioid treatment is effective and requires nonjudgmental treatment providers, family members, and society. One person’s loss is society’s cost. Sometimes, people need more than one treatment for effective results — just like in cancer, and sometimes one treatment can last for years.
If you had cancer, you know that you would go to a doctor and find out what you had to do to stay alive longer. In the same way, if you misuse or overdose on opioids, there is treatment available. We put this module together to guide you through the treatment path. We believe that if you know what’s coming, you can be prepared for it and respond better. If you haven’t taken the quick test, do so now to see where you come out and then decide what you’re going to do with the results. Of course, you can stick your head in the sand and do nothing, and that probably means you’ll continue to struggle. There can be another sunrise to view, another gathering with family to enjoy the holiday, another baby’s smile to see. I can go on.
A treatment plan offers you the chance to think about your problem and learn the skills to reverse your illness. For those who have this illness, it’s time for you to enter treatment and get help for your addiction. Sure, you may have tried it before, and after a while, you went back to drugs. Well, just like cancer treatment, sometimes more than one treatment is required.
Signs of an Opioid or Substance Use Disorder
- A substance use disorder involving opioids causes significant impairment and distress.
- Unsuccessful efforts to cut down or control the use.
- Failure to fulfill obligations at work, school, or home, among other criteria.
- Overpowering desire to use opioids, increased opioid tolerance, and withdrawal when use has stopped.
Substance Use Health Assessment
Answer the questions as completely as possible. At the end, you will be presented with a general assessment of the level of concern you should apply to your substance use.

Time’s up
Opioid Use Disorder:
Causes, Symptoms and Treatment

Source: Medical Centric | https://youtu.be/Fa2XQYHGW5k
Important Things to Know about Treatment
- Treatment must be readily available.
- The earlier the treatment is offered, the better.
- Counseling/behavioral therapies are important.
- Treatment must be continually monitored and followed/linked.
- Mental health issues common in people with Substance Use Disorder should be addressed. Medically assisted detoxification is only the first stage of addiction treatment and does little to change long-term drug use.
- Treatment does not have to be voluntary to be effective.
- Family and peers are important to recovery.
- Many people who misuse opioids do not get treatment. They need to know about treatment options.
- Medications (methadone, buprenorphine, or naltrexone) are helpful.
Understanding Opioid Addiction Treatment and Types of Medications

Source: Mass General Brigham | https://youtu.be/8iwL6R4cczA
When to Seek Professional Help
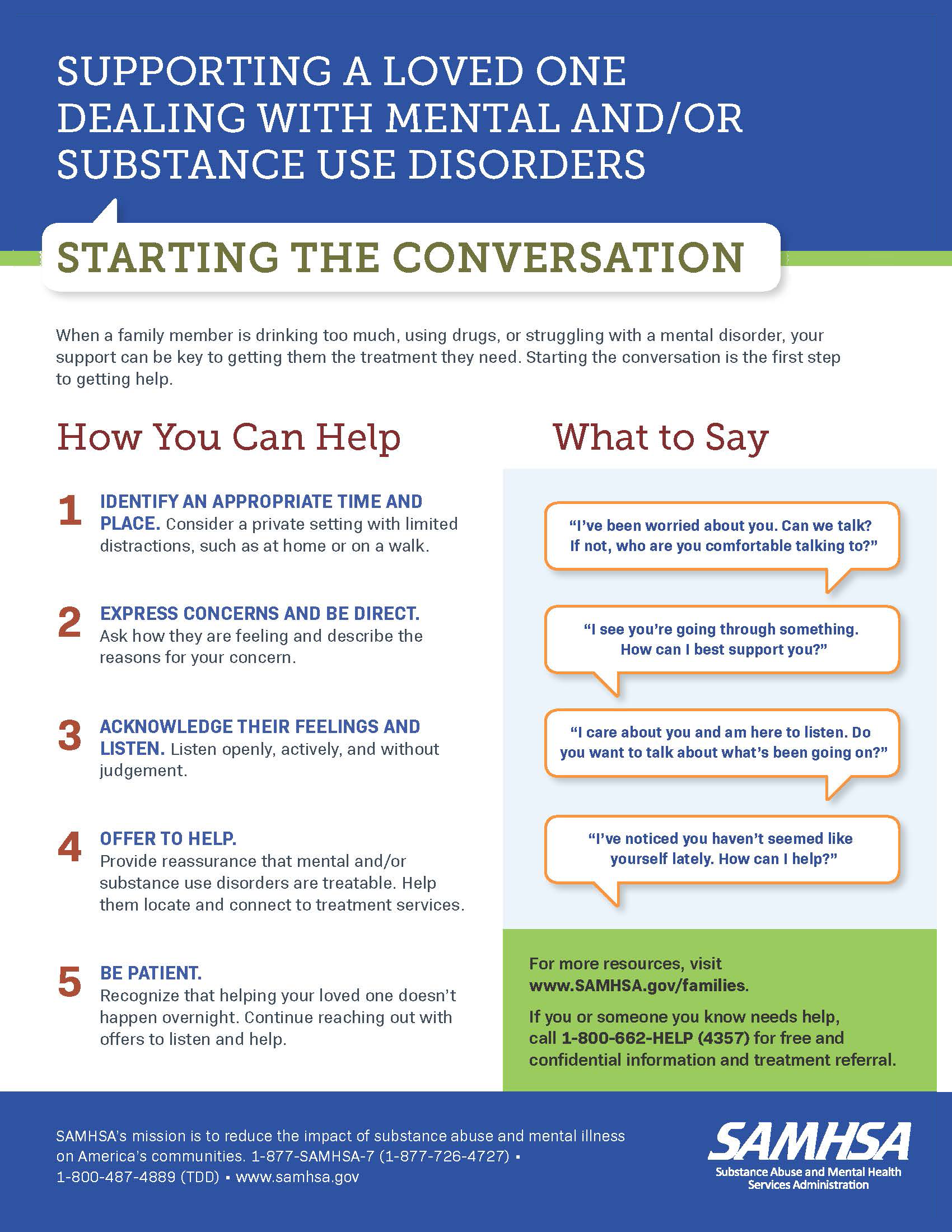
We must work to destigmatize the seeking of professional mental health help and ensure it is available in our community with competent, trained practitioners familiar with and attuned to the racial and ethnic minorities in our community. One of the goals of the group that will work to improve our community might be to assess the availability of affordable mental health treatment, which has implications for MOUD treatment and choice of medication and is of special concern for returning citizens.
Because many people who misuse opioids have accompanying mental health issues, this mental health access is vital, and if available before substance misuse begins, it may prevent or lessen the impact of substance misuse.
We must get the word out to our neighbors and family to seek professional help if you are experiencing severe or distressing symptoms that have lasted two weeks or more, such as:
- Difficulty sleeping
- Appetite changes that result in unwanted weight changes
- Struggle to get out of bed in the morning because of your mood
- Difficulty concentrating
- Loss of interest in things you usually find enjoyable
- Inability to perform usual daily functions and responsibilities
A Recap of the Impact of Opioids
“What causes opioid addiction,
and why is it so tough to combat?”

But there is hope!!!*
“Why Recovering from Opioid Addiction
Is so Difficult | PBS: NOVA, Addiction”
Before you begin treatment here are some things to know:
You must admit you have at least one problem— drugs impairing your ability to function. For example, Black and Latinx groups in the United States, 90% and 92%, respectively, diagnosed with a substance use disorder did not receive addiction treatment (Cruz, 2021). According to federal government data, Black patients are half as likely to be referred to or access treatment even after a nonfatal overdose as non-Hispanic White patients. In another study, results show that Black older adults were 37% less likely to complete a substance use treatment program than Whites. Nearly 90 percent of Black and African American people over the age of 12 with a substance use disorder did NOT receive treatment.
If people do not get treatment, they will raise children whose ACE scores will rise, creating a perpetual cycle of problems.
Stigma gets in the way of connecting and following up with treatment.
How to recognize and overcome stigma that is getting in the way of treatment. Yes, treatment does involve taking another drug instead of the one you’re hooked on. However, treatment involves a plan that is legal and doable.
Stigma is the sense of disgrace, of being outside the bounds of the community. Many Blacks feel that getting mental health help is not part of their culture and something that may cause them shame. The emotional and cultural norm stemming from this belief has harmed people in the Black community who could benefit from professional mental health help and find ways to empower themselves by being able to think and act more clearly. Certainly, the problem with stigma has an impact on substance abuse help. So, to get things in order, we first discuss stigma — what it is and how to get over it. Then, we suggest treatment. If you feel stigma about seeking treatment, then you are unlikely to get it and follow up with it.
Stigma and Treatment: How to Correct

The Substance Abuse and Mental Health Services Administration (Santoro & Santoro, 2021; SAMHSA, 2019) suggests that individuals may be misinformed and/or biased about opioid use disorders. Treatment providers and concerned individuals should provide accurate information about the nature of addiction and the role of brain functioning to address myths and presumptions about addiction and recovery.
It is important to clarify the medical nature of opioid addiction as a chronic illness responsible for hijacking chemicals in the brain. This is a message that should be communicated in counseling sessions and educational sessions in the community.
Addressing Stigma in Healthcare
The NIH HEAL Initiative challenged researchers to consider stigma when planning ways to address the opioid crisis.

How to Provide Support
Recommendations and Resources
Combat MOUD: Myths and Misconceptions
(MOUD)/Medication Assisted Treatment (MAT) is harmful and perpetuates stigma, limiting recovery options and healing. FALSE.
MOUD/MAT just substitutes one addiction for another.
False. MOUD/MAT promotes healing and recovery by relieving withdrawal symptoms and reducing drug cravings. It can prevent relapse without causing a “high” to improve patient survival, increase retention in treatment, decrease illicit opiate use and criminal activity, and increase employment ability and maintenance (National Center on Substance Abuse and Child Welfare, n.d.).
Quitting drugs is all about willpower.
False. Addiction is a medical disease that affects the brain and body. Opioids are highly addictive and change how the brain works. Many treatment programs supplement opioid withdrawal drugs with behavior therapy and/or support groups to address biological symptoms (NIDA, 2018).
You should not be on MOUD/MAT if you are pregnant.
Quickly stopping opioids during pregnancy can have serious consequences, including preterm labor, fetal distress, or miscarriage. Talk with your doctor about which drug is best for you. Women with opioid use disorder may have babies with NAS (Neonatal Abstinence Syndrome) or NOWS (Neonatal Opioid Withdrawal Syndrome). Close collaboration with the pediatric care team can identify and treat NOWS/NAS (SAMHSA, 2018).
MOUD/MAT should not be long-term.
Individuals’ treatment plans are created with their doctors, and the length depends on the person (FDA, 2023). People may safely be on MOUD/MAT medications for months, years, or even a lifetime. Shortening or extending treatment should always be discussed with one’s provider first.
Medication-Assisted Treatment and Common Misconceptions

Source: SAMSHA | https://youtu.be/_RP27Qh1hZY
Steps to Build Family and Community Support
- Raise awareness of Adverse Childhood Experiences (ACEs), which are associated with substance use disorders, including an earlier age of initiating opioid use, recent drug use, and lifetime overdoses (Stein et al., 2017). See Module 3 on ACEs.
- Reduce stigma around seeking help with parenting challenges, substance misuse, depression, and suicidal thoughts.
- Shift the focus from individual responsibility to community solutions and promote safe, stable, nurturing relationships and environments where children live, learn, and play.
Treatment Access
Access and Insurance
Do you have insurance, and do you know where treatment are? Disparities in access to care and treatment for Black and African American people have persisted over time, according to Black Mental Health. Implementation of the Affordable Care Act has helped to close the gap in uninsured individuals, 11.5 percent of Black and African Americans versus 7.5 percent of white Americans were still uninsured in 2018. In 2018, 58.2 percent of Black and African American young adults 18 – 25 and 50.1 percent of adults 26 – 49 with serious mental illness did NOT receive treatment.
Ask your healthcare provider about a full range of options for MOUD (Medications for Opioid Use Disorder) available in North Carolina. The good news is Medicare expansion has passed NC. Medicare probably will pay for MOUD. Know your rights and ask for MOUD treatment if you are eligible.
The Current State of Treatment
How many people with opioid use disorder (OUD) do not receive evidence-based treatment?
90%
What percentage of outpatient treatment programs offer medication for addiction treatment?
27%
What are the barriers to opioid treatment?
Opioid Treatment Has a Racial Component
What Is the Treatment for Opioid Disorder?
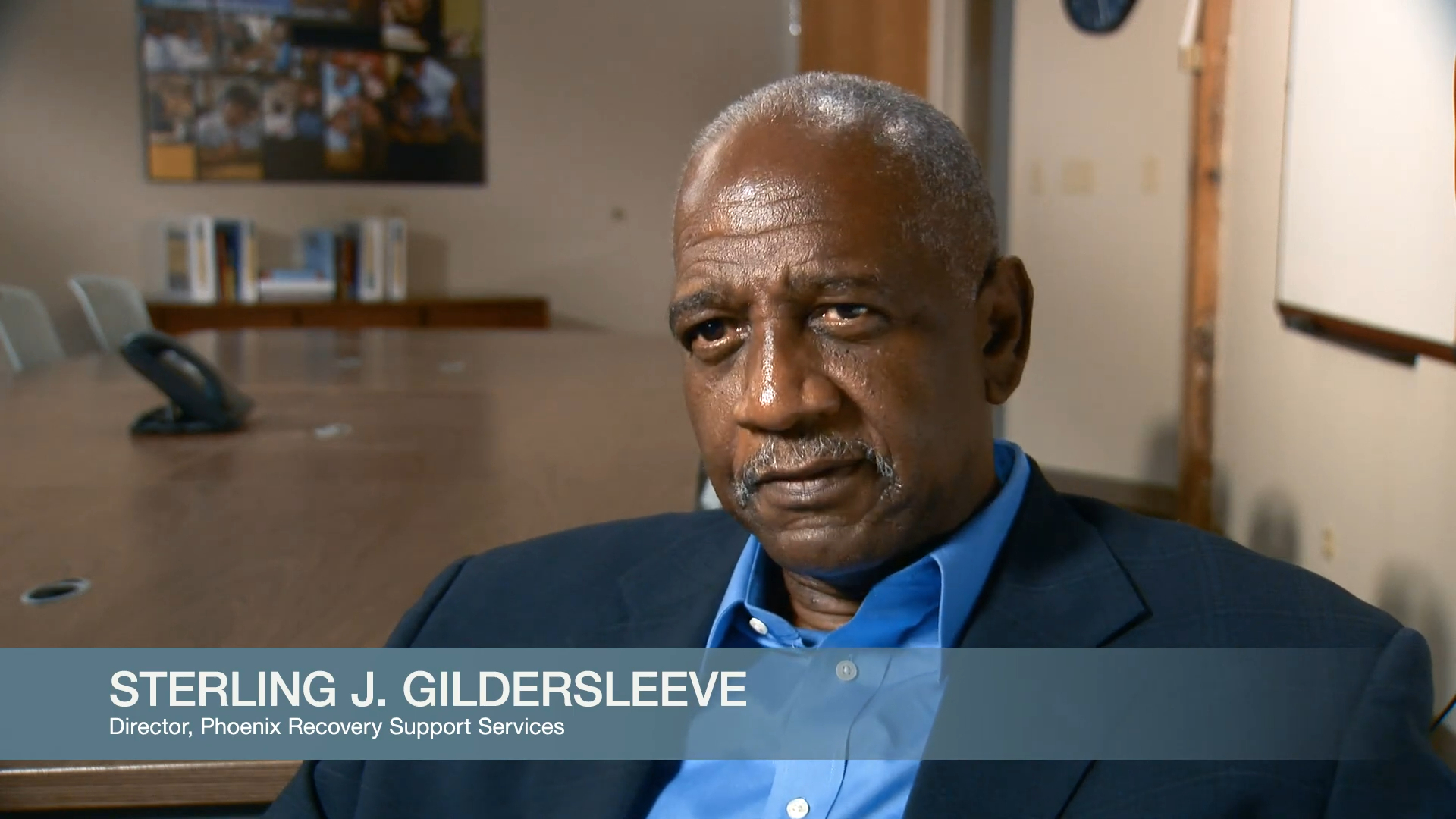
Many Paths to Recovery
One size doesn’t fit all. The are many paths to recovery. Treatment can look different for different people. For example, some get buprenorphine only. That’s all they get. And that’s helpful. Some get that plus counseling. Others get methadone. Some people choose abstinence. Just as there are many roads into overdose, there are many roads out — talk with your health professional and loved ones about what’s right for you.
Elements of an Effective Treatment Plan
Health Resource Guide by Region
Reversing the Epidemic
Integrated Health Care
The best treatment plans may need a variety of professionals:
- Nurses
- Social Workers
- Psychiatrists
- Therapists
- Doctors

- Proper communication among team members
- Respect for the opinions of all healthcare providers involved
- Patient involvement in treatment decisions
- Prioritizing the patient’s needs

Medication for Opioid Use Disorder (MOUD)
MOUD, also known as Medication-assisted Treatment (MAT), is combined with counseling for a “whole-patient” approach and addresses other health conditions, including mental health.
Evidence shows that methadone, buprenorphine, and naltrexone all reduce opioid use and opioid use disorder-related symptoms, and they reduce the risk of infectious disease transmission and criminal behavior associated with drug use. These medications also increase the likelihood that a person will remain in treatment, associated with lower risk of overdose mortality, reduced risk of HIV and HCV transmission, reduced criminal justice involvement, and greater likelihood of employment, according to NIDA. (2021).
FDA-approved Medications for Treating Opioid Use Disorder (OUD)
- Methadone — replacement medication that suppresses or reduces cravings for opioids.
- Buprenorphine — replacement medication, that suppresses or reduces cravings for drugs being misused.
- Naltrexone — blocking medication which binds and blocks opioid receptors for drugs being misused.
Medication-assisted Treatment Options for Opioid Misuse
Methadone | Buprenorphine | Suboxone | Naloxone |
|---|---|---|---|
Full opioid (agonist). Binds fully to mu-opioid receptors, allowing its effects to be fully felt. | A partial mu-opioid agonist, so while it binds to receptors, it does not produce the same intensity of effect as methadone and other full agonists. | Antagonist — meaning that it binds to opioid receptors and can reverse and block the effects of other opioids. | An opioid antagonist, a medication that blocks opiate receptors, therefore blocking the effects of the opioid. |
Methadone is a Schedule II controlled substance, indicating a higher misuse risk. | Buprenorphine is a Schedule III controlled substance with lower risk and generally has fewer requirements. | Suboxone is a Schedule III controlled substance with lower risk and generally has fewer requirements. | Exempt from Drug Enforcement Agency (DEA) scheduling |
Synthetic | Semi-synthetic compound | Synthetic or semi-synthetic Contains both buprenorphine and naloxone – and works to reduce withdrawal symptoms of dependence | Synthetic An antidote to reverse an opioid overdose |
24 to 36 hours or half-life | 36 to 45 hours/half-life | Lasts about 24 hours | 4 mg, and repeat every 2 – 3 minutes in alternating nostrils until help arrives |
Oral concentrate (10 mg/ml), oral solution (5 and 10 mg/5ml), tablet (5, 10, and 40 mg), injection (10mg/ml) and powder (50, 100, and 500 mg/bottle for prescription compounding). | Oral forms include a buccal film and sublingual tablets. Parenteral routes include a subdermal or subcutaneous implant and intravenous (IV) or intramuscular (IM) injections. | Film dissolved in the mouth Oral Pill Injection in the stomach | Nasal spray Injection |
Higher risk of overdose- Need more supervision, more highs | Less risk of overdose due to the ceiling effect | Less risk of overdose due to the ceiling effect | No risk
|
Providers who have completed special certification through clinics Specialized Opioid Treatment Program (OTP) license | Any physician can prescribe buprenorphine in NC, but X‑waiver for advanced practice providers (PAs ) require them to take special training. Easier to access than methadone | Doctors apply for specialized certification | Anyone can administer Narcan/Naloxone |
It can take weeks to reach a full therapeutic effect with methadone | It takes only a few days with buprenorphine to reach full effect. | It takes effect in about 20 to 60 minutes. | It takes effect in a couple of minutes (2 – 3) and lasts for about 30 to 90 minutes. |
Moderate to severe protracted withdrawal systems/ fewer side effects | Mild withdrawal symptoms/more side effects | May result in acute withdrawal | withdrawal symptoms may last as long as a month |
Inexpensive | More expensive than methadone | More expensive than methadone | The nasal spray is more expensive than the injection. |
Table references: Notes for this chart are in Appendix A with references for Module 5.
Medication-Assisted Treatment Overview: Naltrexone, Methadone & Suboxone l The Partnership
Mechanism of Action of a Partial Opioid Agonist
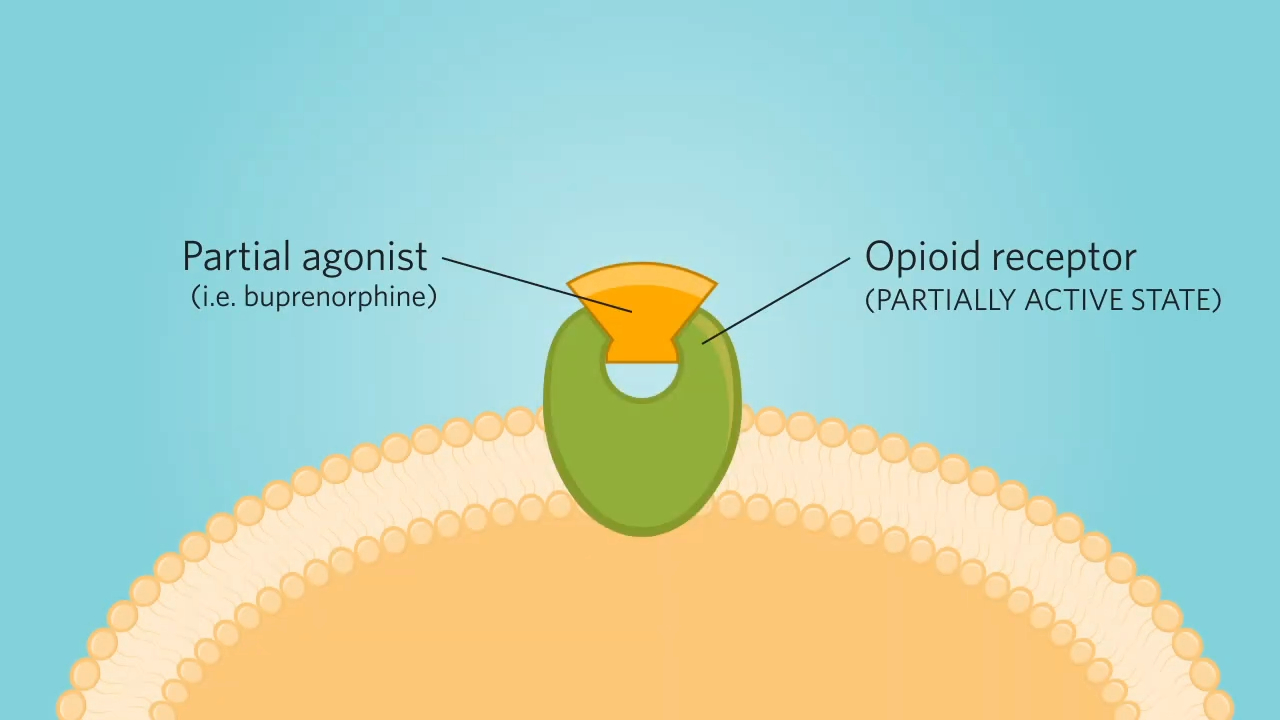
How Does Medication Work?
Medical Intervention
Health problems are frequent in individuals with SUD including HIV, hepatitis A, B, & C. Sexual side effects are also common. Other chronic health conditions such as lung disease, heart disease, cancer, and other illness may exacerbate the problem. They must be addressed concurrently, using a whole-person approach.
Overdose risk factors
- Mixing opioids with respiratory depressants or “downers” such as alcohol or benzodiazepines.
- Mixing opioids with stimulants or “uppers” such as cocaine or methamphetamine.
- History of past overdoses.
Source: Opioid Overdose Risk Factors (Mass.gov)
Housing Intervention
Participants noted that being discharged to live on the streets or to a shelter without placement in a recovery house created many challenges and that many people face triggers for their opioid use when they do not have a place to go after inpatient detox (David et al., 2022).
Some participants reported that without a plan in place, they were unable to get the support they needed to successfully complete crucial next steps on the road to long-term recovery (David et al., 2022).
Some participants identified safe and stable housing as an important factor for success and discussed using treatment to get help with housing instability. Assistance in securing stable housing would allow individuals to focus on recovery from substance use (David et al., 2022).

Connection Between Homeless Problem and Drug Addiction in USA

Source: Our 50 States | https://youtu.be/yiRK5f_mWkc
Mental Health Intervention
About 51.4% of the total opioid prescriptions distributed in the United States each year were written for people with a history of anxiety or depressive disorders, (Davis, Lin, Liu, & Sites, 2017).
Those who are suffering from pain often have anxiety and depression. Many struggle to cope with daily stressors or past trauma. Mental health therapy can help a person:
- Become motivated to change
- Develop an understanding for why we misuse substances
- Develop problem-solving skills
- Help reduce or stop drug misuse
- Replace drug use with new healthy activities
- Refine or develop effective skills for rebuilding relationships
- Build a support network
- Group therapy can help you know that you are not alone
Peer support programs can help maintain abstinence.
Introduction to Cognitive Behavioral Therapy
for Substance Use Disorders

Source: Friends & Supporters| https://youtu.be/Otu5Ajlo-_w
Harm Reduction
- Meets people who use drugs (PWUD) where they are at
- Aims to prevent overdose and infectious disease transmission
- Offers low-threshold options for accessing substance misuse treatment and other health care services
- Emphasizes the need for humility and compassion toward those who use drugs
- Helps prevent acute life-threatening infections related to nonsterile drug injection and chronic diseases like HIV
Fentanyl test strips (FTS) can detect the presence of fentanyl in drug samples before use.

Sources:
Centers for Disease Control (CDC), National Harm Reduction Technical Assistance Center. https://harmreductionhelp.cdc.gov/s/
Krawczyk, N., et al, 2022. “Intersecting substance use treatment and harm reduction services: exploring the characteristics and service needs of a community-based sample of drug users.” Harm Reduction Journal, 19(1).
Substance Abuse and Mental Health Services Administration (SAMHSA) (April 24, 2023). Harm Reduction. https://www.samhsa.gov/sites/default/files/harm-reduction-framework.pdf
Harm Reduction Principles: Ryan White HIV/AIDS Program TargetHIV. https://www.youtube.com/watch?v=UXdLsyuQATk
Post-overdose Response Team (PORT)
The overdose follow-up program allows agencies to visit a recently overdosed person (within 24 – 72 hours). According to the North Carolina Harm Reduction Coalition (NCHRC), a follow-up visit within days of a naloxone reversal provides the following:
- Opportunity to direct people to harm reduction services and/or treatment to reduce or stop substance use.
- Opportunity to provide naloxone, overdose prevention training, and prevention materials.
- Opportunity for stakeholders to work together to reduce overdose mortality.
Source: North Carolina Department of Human Services: Post Overdose Response Toolkit (PDF)
Relapse Prevention Strategies Help People Stay in Treatment
Top Relapse-Prevention Strategies
- Self-care
- Address common withdrawal symptoms including insomnia and fatigue
- Assess HALT (Hungry, Angry, Lonely, and Tired)
- Practice Mindful Meditation
- Identify Your Triggers
- May include boredom, stress, money problems, relationship issues, certain sights or smells, certain people or places, falling into old habits, anger, etc.
- Join a Support Group, either online or in-person
- Use Grounding Techniques
- Breathe Deeply
Source: Parisi, Theresa, “The Top 10 Relapse Prevention Skills,” October 24, 2019. Addiction Center.
Complementary/Alternative Health Approaches for Chronic Pain
Rather than taking opioids to treat chronic pain, a person may try other ways to reduce pain such as acupuncture, hypnosis, massage, mindfulness meditation, music-based interventions, spinal manipulation, tai chi, qigong, and yoga.
- Some people have found relief by using the TENS unit (TENS, NHS, 2022). Transcutaneous electrical nerve stimulation (TENS) is an easy-to-use pain relief method using a mild electrical current connected to sticky pads (electrodes).
- To learn more about chronic pain alternative treatments, visit: https://www.nccih.nih.gov/health/chronic-pain-what-you-need-to-know#hed3
- For dietary supplement recommendations, visit https://www.nccih.nih.gov/health/dietary-and-herbal-supplements
Transportation to Treatment
Modes of transportation within Durham County include:
- GoDurham and GoTriangle (Public Transportation in Durham County through both fixed-route bus service and ACCESS demand-response van service) 919 – 485-RIDE.
- GoDurham ACCESS (Durham County contracts to provide transportation options for qualified individuals for medical, employment, human services, government, and personal care trips).
Wisdom Care Transportation (specializes in Non-Emergency Medical Centers Transportation) needs, from airport transfers to transportation to medical, chemotherapy, dialysis, adult day centers, etc. Medicaid accepted.
Duke Regional: (919) 470‑4000 Duke ER only does referrals and assessments.
NC Specialty Hospital: (919) 514‑1700.
Lincoln Community Health Center: (919) 956‑4000
Don’t Wait until Symptoms Are Overwhelming
Talk about your concerns with your primary care provider, who can refer you to a mental health professional, if needed. If you don’t know where to start, read the National Institute of Mental Health (NIMH) Tips for Talking With a Health Care Provider About Your Mental Health. Learn more about how to get help or find a provider from the National Institute of Mental Health. This advice is especially critical for people in minority communities where there is still a stigma regarding seeking help for mental health.
Corporations are becoming increasingly aware of the problem. Blavity, Inc., a public relations firm, is concerned with Black mental health, and on their website, they urge companies to promote the issue and solutions. They quoted some statistics: from Mental Health America: “Of the 13.4% of the U.S. population identifying as Black or African American, 16% reported having a mental illness within the past year alone. For context, 16% of the Black and African American population in the United States amounts to well over 7 million people…While factors such as poverty, racism, and violence take a toll on Black people’s mental health and wellness, issues such as generational trauma and maternal mental health also plays a role.” https://blavity.com/studies-back-up-fact-that-generational-trauma-has-detrimental-impact-on-mental-health-of-black-youth
They are part of companies stepping up to make a difference. Our role will be to interest other companies and services to take an interest in the issue and work with us to reduce ACEs.
What to Do in a Crisis – Suicide Concerns
Along with the growing substance misuse epidemic, there is also a suicide epidemic, and often they stem from the same sources.
There is help.
- If you or someone you know is struggling or having thoughts of suicide, call or text the 988 Suicide & Crisis Lifeline at 988 or chat at 988 Lifeline Chat.
- This service is confidential, free, and available 24 hours a day, seven days a week.
In life-threatening situations, call 911.