Preventing Opioid Deaths: Availability and Use of Naloxone
Medication is available that can counteract an opioid overdose, and it can help save lives. Carry and learn how to use naloxone/Narcan in the event you are nearby when someone has had too much heroin, fentanyl, or any prescription opioid medication.
The opioid crisis is devastating, but we have ways to reduce its impacts, including the death rate. Please prevent opioid misuse; share information about opioid treatment; carry Narcan; seek treatment; and pledge to inform others.
What Is Naloxone?
Definition
Naloxone is a life-saving medication that can counteract an overdose of opioids, including heroin, fentanyl, and prescription opioid medications. Naloxone/Narcan is available in most states without a prescription, is easy to use, and light to carry. Carrying naloxone with you can help save lives (CDC, 2023).
Naloxone is now available over the counter at Walgreens, other drug stores, and at some local grocery stores. It’s about $45/two doses. However, it is free in two Durham locations.
One is at the local Durham County Detention Center, 219 S Mangum St, Durham, NC 27701 which is open 24/7 and another is free at the Durham County Public Health Center at 414 E Main St, Durham, NC 27701 during business hours.
All K‑12 public schools in Sacramento, California, have Narcan available. Also, White House Urges Schools to Carry Naloxone, the Opioid Overdose Treatment (MedicineNet.com). See if your local school carries Narcan, and if they do not, urge them to do so.
- Bystanders with naloxone can help save the life of a person who has overdosed on opioids.
- Those struggling with opioid use disorder (OUD) should carry naloxone and keep it at home. (80 percent of overdose deaths occur at home).
- Because you can’t use naloxone on yourself, let others know you have it in case you experience an opioid overdose.
- Carrying naloxone is especially recommended for people who are taking high-dose opioid medications (greater or equal to 50 morphine mg equivalents per day), people who use opioids and benzodiazepines together, or people who use illicit opioids like heroin.
What Is Opvee?
Definition
Opvee is a new prescription nasal spray that is more effective than Narcan, especially with fentanyl overdoses. It’s stronger and lasts longer but has more side effects.
For more information: “Opvee vs. Narcan: 6 Similarities and Differences Between These Opioid Reversal Medications” from Good RX Health by Jennifer Gershman (September 2023).

Resources
Preventing Drug Overdoses and Deaths
WATCH AND DISCUSS
Overdose Prevention Video (5 min.)
from the National Institutes of Health and the National Institute on Drug Abuse
Recognizing Signs of an Opioid Overdose and How to Respond
What Happens During an Overdose?
Death from an opioid overdose happens when too much of the drug overwhelms the brain and interrupts the body’s natural desire to breathe. During an overdose, breathing can be dangerously slowed or stopped, causing brain damage or death.
5 Signs of an Opioid Overdose
Recognizing Signs of an Overdose
Responding to an Overdose
Hover over the cards below for more instructions.
STIMULATION
If there is a response, keep the person awake until help arrives.
CALL FOR HELP
Say: “A person has overdosed or is unresponsive.”
RESCUE BREATHING
GIVE NALOXONE
RECOVERY POSITION
DON’T Take Drugs Alone
Street drugs do not go through FDA testing for purity, so when you take street drugs, you don’t know what you’re getting or how strong the impact will be. Many people use opioids in combination with other drugs and alcohol, increasing their lethal impact. Using opioids when you are alone increases your risk of death because if your breathing stops or you get ill, no one is there to save you by administering naloxone, and you can’t give yourself naloxone. Check out Survival Strategies While Using Drugs Alone from People Who Use Drugs by People Who Use Drugs. PWUD-ServiceProvider-Guide-07142021.pdf (vitalstrategies.org) Read what they suggest and see if it makes sense.
How to Spot Someone
So They Never Have to Use Alone

Source: Canadian Association of People Who Use Drugs.
https://www.youtube.com/watch?v=KbUwb-pszW4&t=170s
Risk Factors
Several factors can increase a person’s risk of overdosing.
- Changes in tolerance may occur after not using opioids or using less of them, such as after in-patient treatment or incarceration.
- Changes in the drug supply.
- Mixing opioids with respiratory depressants or “downers,” such as alcohol or benzodiazepines (benzos), can slow down the central nervous system and can lead to extreme sleepiness, slow or difficulty in breathing, coma, or even death (Vermont Department of Health, n.d.).
- Mixing opioids with stimulants, such as cocaine and methamphetamine.
- Having chronic health conditions such as HIV, Hepatitis C, lung disease, heart disease, or other health concerns.
- History of past overdoses.
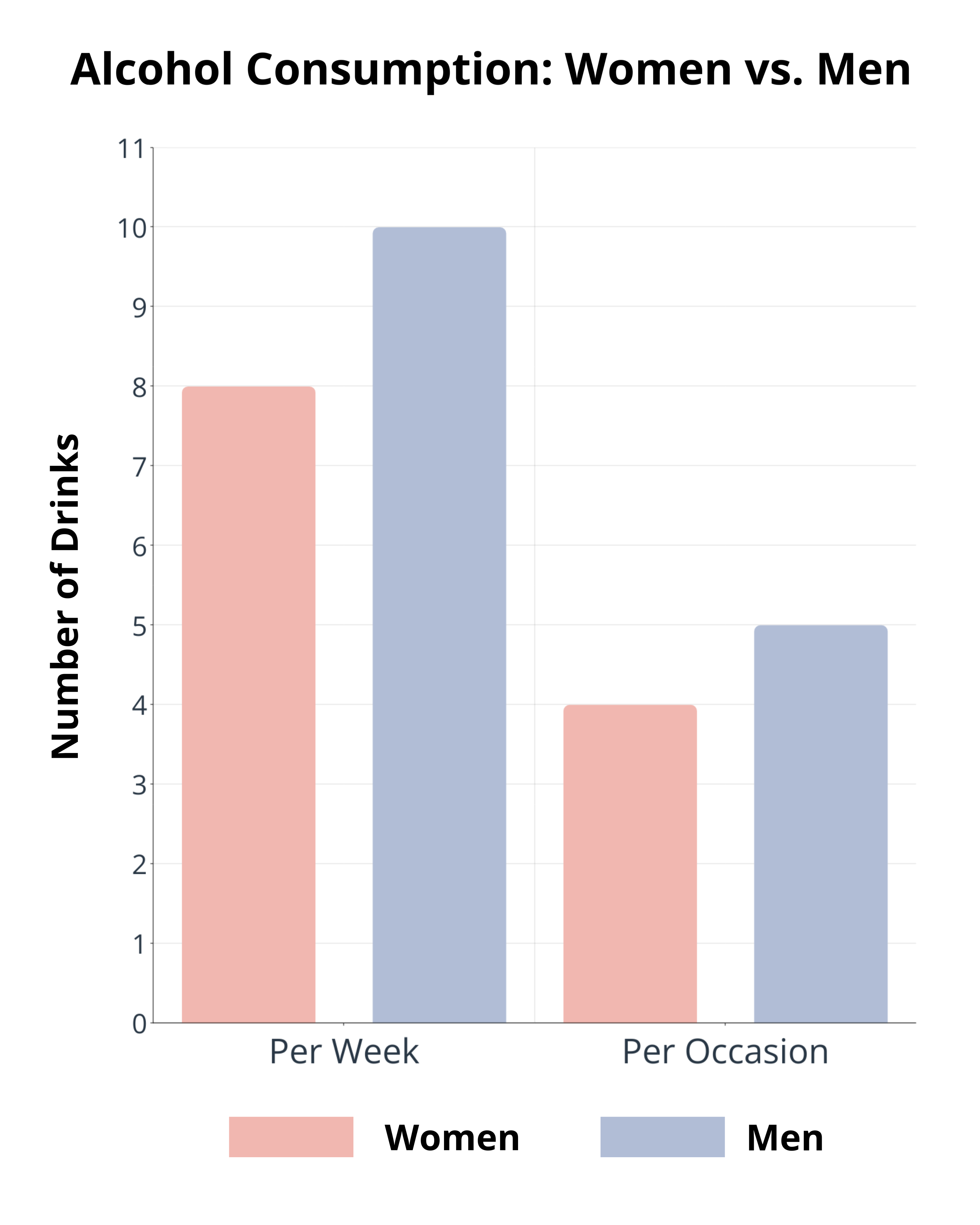
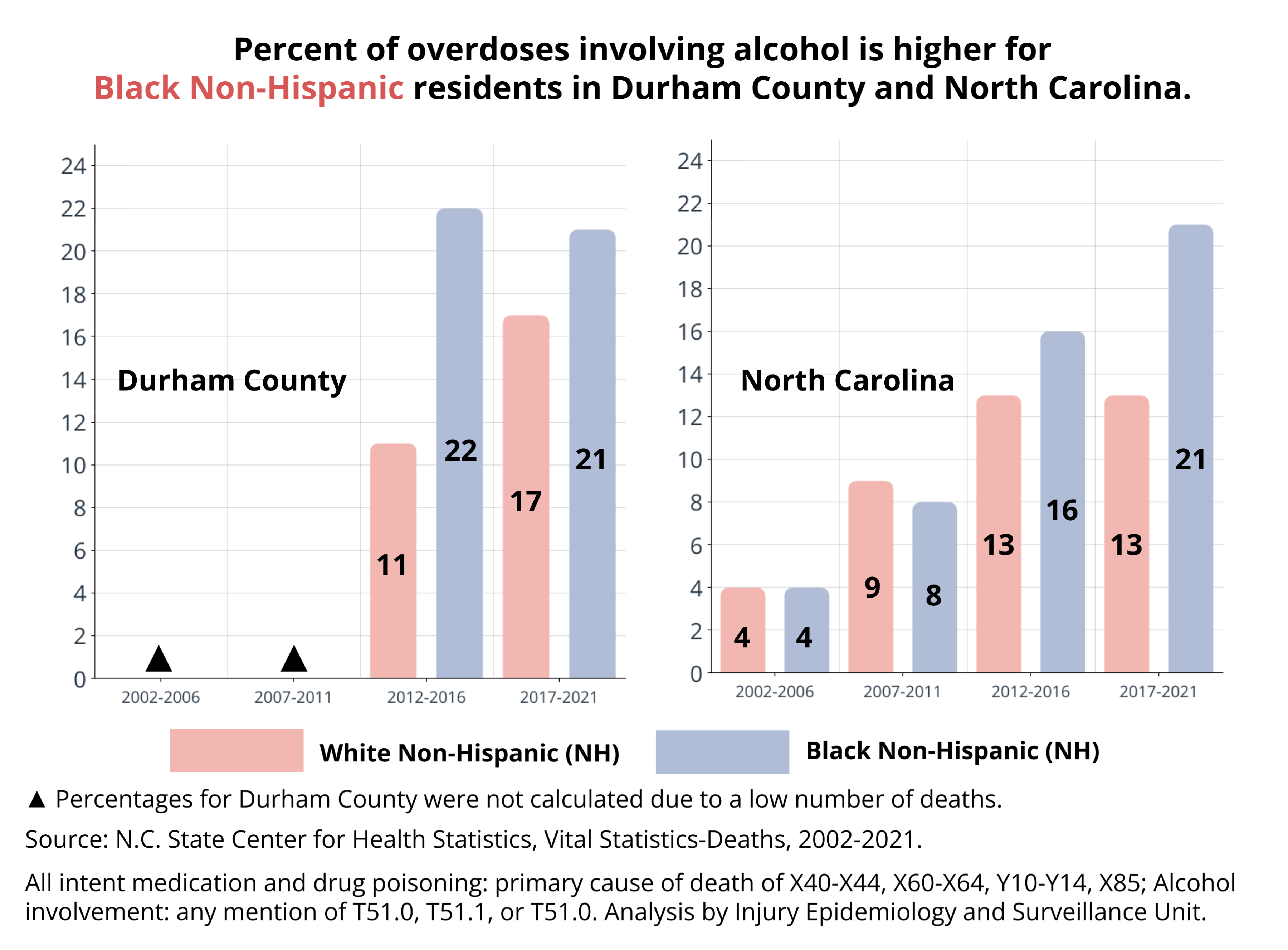
Alcohol and Opioids: A Deadly Combo
A person who misuses alcohol has a greater risk of using at least one other substance, such as opioids, marijuana, cocaine, and heroin. Prolonged use of drugs and alcohol increases your tolerance, requiring more substances to achieve the same effects (Alcohol Rehab Guide: Recognizing a Drug and Alcohol Problem, May 2023).
Opioids and alcohol are both depressants that slow down breathing and impair judgment. Mixing them has a synergistic effect, meaning each substance is stronger when taken together than when taken separately, often leading to potentially fatal consequences, such as coma, brain damage, overdose, and death. Therefore, no amount of alcohol is considered safe when taking opioids.
Don’t mix depressants (aka downers), including alcohol, opioids (heroin, morphine, oxycodone, hydrocodone, fentanyl), and benzodiazepines. Depressants can slow your breathing and increase your risk of death and other bad outcomes, such as damage to your brain and other organs. In other words, DON’T DRINK WHEN YOU TAKE OPIOIDS.
Mixing stimulants and depressants does not balance or cancel each other out. The results of combining drugs are unpredictable, often modifying or even masking the effects of one or both drugs, which may trick you into thinking that the drugs are not affecting you, making overdosing easier.
Opioids + alcohol = BAD RESULTS
- Respiratory depression and arrest
- Unconsciousness
- Cardiovascular risk
- Irregular heart rate
- Coma
- Nausea and vomiting
- Dehydration
- Changes in blood pressure
- Loss of coordination
- Dizziness
- Extreme lack of inhibition
- Unusual behavior
- Death
Stimulants (also known as Uppers) include Ecstasy (MDMA), cocaine, methamphetamines, and amphetamines (speed).
Source: Geng, Caitlin. (2022, Dec 7). What to know about alcohol and opioids. Medical News Today. Alcohol and opioid use: Risks, side effects, and more (medicalnewstoday.com)
Stimulants + opioids =
- Fast/troubled breathing
- Increased body temperature
- Nausea or vomiting
- Chest pain
- Seizures or tremors
- Brain injury
- Liver damage
- Heart attack
- Stroke
- Death
Source: American Psychiatric Association (2022), Diagnostic and Statistical Manual of Mental Disorders (DSM), 5TR text revision. American Psychiatric Association, 2022.
Standard Drink Sizes
5% ABV beer
7% ABV malt liquor
12% ABV wine
40% ABV distilled spirits
What Is Excessive Alcohol Consumption?
Alcoholic beverages should not be consumed by pregnant persons and those under age 21.
Speedballing
Speedballing is taking cocaine and heroin together which causes a “push-pull” reaction in the body that can be very dangerous. It is especially risky because it forces the body to process more types of drugs simultaneously.
What You Need to Know about Providing Medical Assistance
Under North Carolina’s Good Samaritan Law, you may not be prosecuted for certain drug offenses under the following conditions.
- You seek medical assistance for someone experiencing a drug-related overdose by contacting the 911 system, a law enforcement officer, or emergency medical services personnel.
- You are the first person to seek medical assistance for the overdose victim.
- You provide your name to the 911 system or a law enforcement officer upon arrival.
- Law enforcement officers were not already at your location executing an arrest warrant, search warrant, or other lawful search.
- Any evidence for prosecution of a drug-related offense obtained by a law enforcement authority was obtained because you sought medical assistance for a drug-related overdose.
Protect Friends and Family with Lifesaving Naloxone (CDC)

You Need to Know
Barriers to access include cost/affordability ($45-$150), insurance coverage, and access, among others.
Fentanyl Test Strips (FTS)
Fentanyl test strips can detect the presence of fentanyl in drug samples. FTS are a reliable means of providing people at risk of fentanyl exposure with more information, which can decrease the risk of overdose. They cost $1 or $2 per strip, but may be free from local health departments.
FTS may be obtained at your local health department, needle-exchange programs (that distribute clean syringes) in your community, and/or vending machines in some states.
Use instructions: Dip the BTNX strip into a sample of the drug dissolved in water. One line indicates that fentanyl is present. Two lines mean it is negative for fentanyl. (No line means the test is invalid).
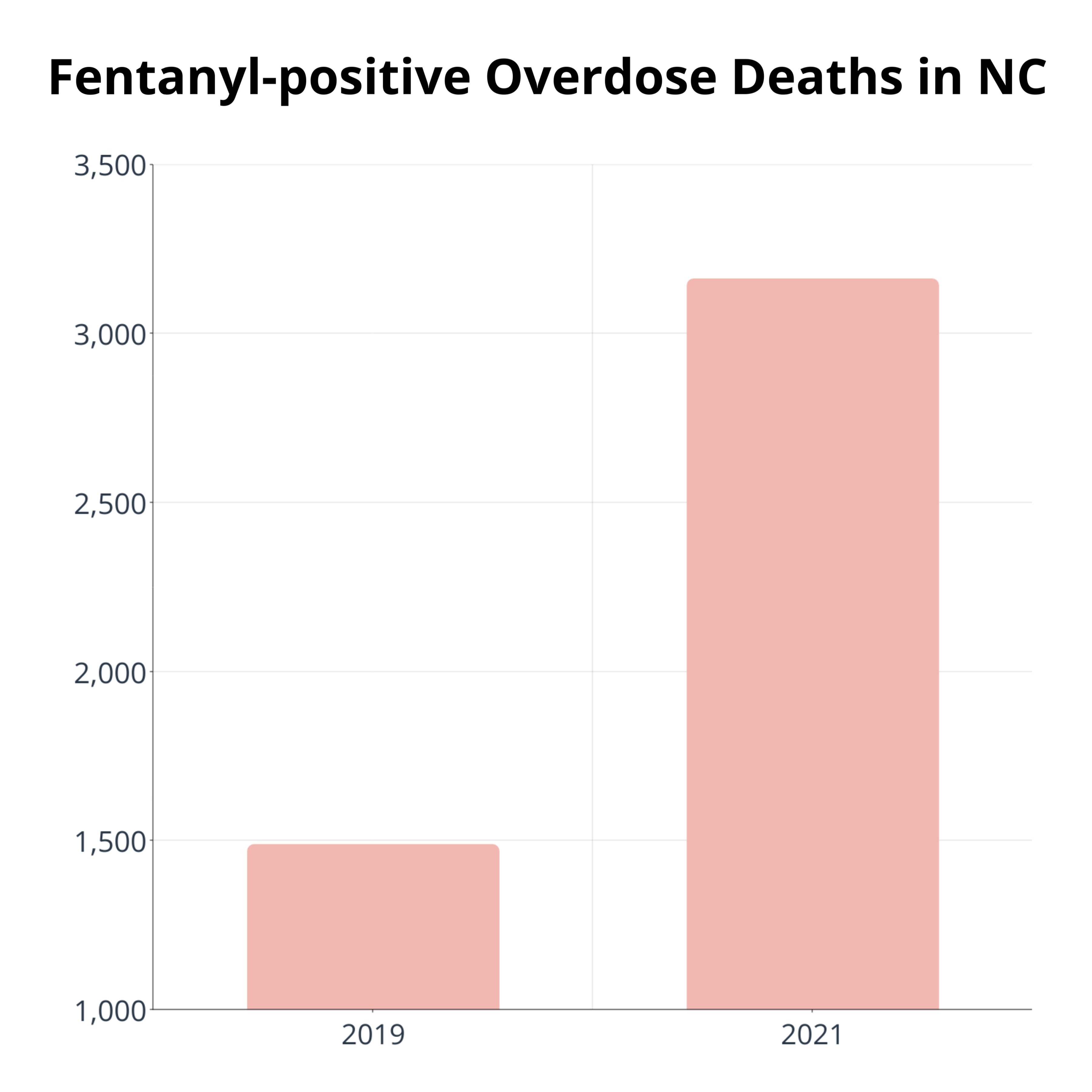
In North Carolina (NC), fentanyl-positive overdose deaths increased by 212% from 1,490 deaths in 2019 to 3,163 deaths in 2021.
Source: “North Carolina pharmacists’ willingness to sell fentanyl test strips: a survey study.” by G.T. Marley, B. Ostrach, & D. Carpenter in Harm Reduction Journal, January 2023
How to Use Fentanyl Test Strips

Please make sure test strips are legal in your state. Otherwise, they could be considered drug paraphernalia.
Where can I get more info about Naloxone?
- North Carolina Harm Reduction Coalition: naloxonesaves.org
- More Powerful NC: https://www.morepowerfulnc.org/.
- National Institute on Drug Abuse (NIDA). (January 2022). Naloxone Drug Facts https://nida.nih.gov/publications/drugfacts/naloxone
- Centers for Disease Control. (April 21, 2023). Life Saving Naloxone. https://www.cdc.gov/stopoverdose/naloxone/index.html
- Centers for Disease Control. (July 10, 2020). Save a Life from Prescription Opioid. Rx. https://www.cdc.gov/rxawareness/prevent/
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2023). What is Naloxone? https://bit.ly/3RHSIkz
- Drug Enforcement Agency. (n.d.). One Pill Can Kill; Save Lives with Naloxone. https://www.dea.gov/onepill/save-lives
- National Institutes of Health and National Institute on Drug Abuse, (n.d.). Overdose Prevention Education for Clinicians Treating Patients with Opioid Disorders. https://youtu.be/7p_SU6zcvbA?t=15
Resources and Sources of Help
Opioids with FDA-Approved Labeling Describing Abuse-Deterrent Properties (CDC, 2021)
FDA has approved these opioids with labeling describing abuse-deterrent properties consistent with the FDA’s Guidance for Industry: Abuse-Deterrent Opioids – Evaluation and Labeling:
Test Your Knowledge (answer yes or no)
1. You need a prescription to obtain naloxone (Narcan).
NO: You can now buy naloxone from a pharmacy without a prescription from a doctor.
2. Pinpoint pupils, slow breathing, and pale or blue skin are all symptoms of an overdose.
YES: More symptoms include choking, loss of consciousness, and a limp body.
3. Even prescription opioids can be dangerous, and anyone can become addicted.
YES: Even when taken as directed, opioids are highly addictive.
4. It is safe to take opioids with other drugs.
NO: Taking opioids along with any other drugs, especially muscle relaxants or sleep drugs, is extremely hazardous and could cause death.
5. Some side effects of taking opioids are increased pain sensitivity, constipation, nausea, vomiting, and depression.
YES: Opioids come with a slew of dangerous side effects that must be carefully monitored.
Thank you for visiting our website.
If you would like to learn more about our research, desire training,
or a presentation at your organization, please contact the PI:
Dr. Dasherline Cox Johnson, Psy.D.
Biomedical/Biotechnology Research Institute (BBRI)
North Carolina Central University
Email: djohn410@nccu.edu
Thank you!